Limberg's technique dates back to the Soviet oral and maxillofacial surgeon Alexander Limberg, who began performing his surgical technique in the 1960s to treat soft tissue defects in the face. The technique was first used in 1986 in a patient with a pilonidal fistula.
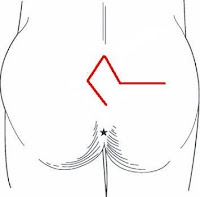
In Limberg plastic surgery, the fistula system is cut out in the shape of a rhomboid and the defect is covered with an adjacent tissue flap, which is also mobilized in the shape of a rhomboid, thus closing the wound. As with the Karydakis and cleft-lift procedures, the gluteal fold is flattened, the sutures are located outside the fold.
 |
| Limberg´s technique |
Limberg's technique is the best-analysed plastic surgical technique for the treatment of the pilonidal disease. Wound healing disorders are not uncommon in the original Limberg technique, which is why the procedure is nowadays usually performed in a slightly modified form, which has reduced the rate of healing disorders to 5 to 15%. The recurrence of pilonidal cyst and tailbone fistula is observed in about 6% of cases. The duration of incapacity to work is 1 to 3 weeks in most studies.
A major disadvantage of Limberg´s technique is the extensive permanent scarring, which more than 60% of patients in studies claim to be cosmetically disturbing. Here, the Karydakis technique performs much better.
 | |
|
In practice, Limberg's technique can be used for the surgical treatment of pilonidal disease, as it has a relatively low recurrence rate (renewed fistula formation) and an acceptable frequency of wound healing disorders. It performs better than traditional fistula cutting techniques. However, there are no clear advantages over the Karydakis technique and the cleft-lift procedure according to Bascom.
Literature sources:
Chijiwa T, Suganuma T et al (2006) Pilonidal sinus in Japan maritime self-defense force at Yokosuka. Mil Med 171:650–652
Gwynn BR (1986) Use of the rhomboid flap in pilonidal sinus. Ann R Coll Surg Engl 68:40–41
Akca T, Colak T et al (2005) Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg 92:1081–1084
Altinli E, Koksal N et al (2007) Impact of fibrin sealant on Limberg flap technique: results of a randomized controlled trial. Tech Coloproctol 11:22– 25
Arslan K, Said Kokcam S et al (2014) Which flap method should be preferred for the treatment of pilonidal sinus? A prospective randomized study. Tech Coloproctol 18:29–37
Cihan A, Mentes BB et al (2004) Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgery. ANZ J Surg 74:238–242
Hegele A, Strombach FJ et al (2003) Plastisch-chirurgisches Therapiekonzept des infizierten Sinus pilonidalis. Chirurg 74:749–752
Jaschke CW, Mährlein R et al (2002) Ergebnisse der Behandlung des Sinus pilonidalis durch Schwenklappenplastik nach Limberg. Zentralbl Chir 127:712–715
Jonas J, Blaich S et al (2000) The Limberg transposition flap in surgical therapy of chronic pilonidal sinus. Zentralbl Chir 125:976–981
Müller K, Marti L et al (2011) Prospective analysis of cosmesis, morbidity, and patient satisfaction following Limberg flap for the treatment of sacrococcygeal pilonidal sinus. Dis Colon Rectum 54:487–494
Ates M, Dirican A et al (2011) Short and longterm results of the Karydakis flap versus the Limberg flapfor treating pilonidal sinus disease: a prospective randomized study. Am J Surg 202:568–573
Karakayali F, Karagulle E et al (2009) Unroofing and marsupialization vs. rhomboid excision and Limberg flap in pilonidal disease: a prospective, randomized, clinical trial. Dis Colon Rectum 52:496–502
Cihan A, Ucan BH et al (2006) Superiority of asymmetric modified Limberg flap for surgical treatment of pilonidal disease. Dis Colon Rectum 49:244–249
Bessa SS (2013) Comparison of short-term results between the modified Karydakis flap and the modified Limberg flap in the management of pilonidal sinus disease: a randomized controlled study. Dis Colon Rectum 56:491–498
Eryilmaz R, Sahin M et al (2003) Surgical treatment of sacrococcygeal pilonidal sinus with the Limberg transposition flap. Surgery 134:745–749